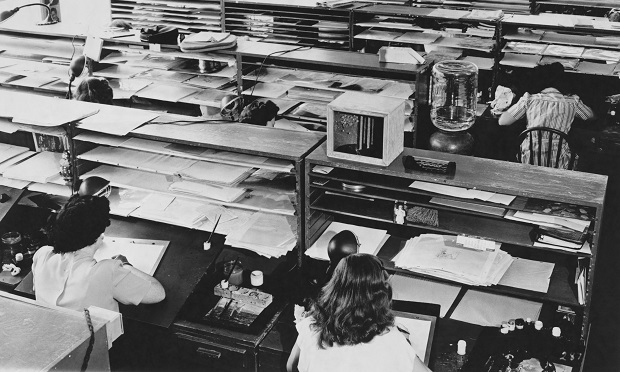
 Utilizing health benefits as an incentive allowed the earliest adopters of this strategy to differentiate themselves from their competitors and begin bringing in the top talent needed. (Photo: Shutterstock)
Utilizing health benefits as an incentive allowed the earliest adopters of this strategy to differentiate themselves from their competitors and begin bringing in the top talent needed. (Photo: Shutterstock)The modern, American employer is expected to offer health insurance, life insurance, dental insurance, retirement accounts, flexible spending and/or health savings accounts, paid vacation and sick time, paid holidays, paid medical leave, and so much more. Entire industries full of vendors, subject-matter-experts, and other stakeholders have popped up to handle the benefits expectations placed on the American employer. This article and its readership serve as an example of the footprint and impact that the benefits industry has had across our general economy for many years.
But how did this come to be? When and why did the modern employer begin this standard offering of benefits? Was it always this way?
Related: Lessons from COVID: Health care needs to get back to basics
Many years ago I was fortunate to work under the tutelage of one of the most influential business mentors I would ever encounter. I was too young and inexperienced to fully appreciate the lessons I was learning at the time, but as I write this article, today, I remember that it was this mentor who first opened my eyes to the idea that the current landscape of employer-sponsored health benefits had not always been the standard. My mentor explained to me that the modern era of the employer-sponsored health plan started to take flight following World War II. I learned of federal legislation called the Stabilization Act of 1942.
Apparently, this Act was passed to help combat inflation during the tumultuous economic times of World War II. Within the Stabilization Act was regulation that limited an employer’s ability to raise salaries and/or wages. As employers realized they were not able to compete for top labor by offering higher pay, those same employers needed to turn to other, newer incentives to attract top talent. The first new incentive that innovative employers started to offer was the employer-sponsored health plan – health benefits! Utilizing health benefits as an incentive allowed the earliest adopters of this strategy to differentiate themselves from their competitors and begin bringing in the top talent needed.
From there it was off to the races in terms of employer incentives and innovative offerings. From the end of World War II through modern times, the suite of offerings has grown to include everything from dental insurance, to disability, to retirement, and so much more, as discussed earlier. Fast forward to 2020 and we have a full, robust set of employer offerings that have become standard fare in almost every sector.
Viewing health benefits through this historical lens can help shift the definition of what might be considered “innovative” in our space and/or what might be considered “important.” Recalling that employer-sponsored health benefits first came to about as an incentive to attract talent, it is worth realigning our discussion on what is innovative and important in the health plan space.
What if we all agreed that the most important and most innovative trend in the health plan space was to offer the most robust benefits possible at the lowest cost possible? A true attractant for the top employee. What if we went so far as to wonder if a robust health plan could be offered to hard-working employees and their families… for free? Could this be the most innovative and important trend in the health plan space? It certainly could become the difference in attracting and retaining top talent, especially considering the expectation of benefit offerings becoming par for the course across employment opportunities – could the cheapest yet richest health plan be the key differentiator in the labor market? Perhaps.
Nothing is free
Now, obviously, nothing is “free.” Costs must be born somewhere. Health claims must be paid and the multiple vendor solutions that assist in the operations and execution of a health plan are not complimentary. So how might an employer create this robust plan at minimal cost to its employees?
Self-funding
This is not an article meant to dive into the fundamentals of what self-funding is and/or how to appropriately go about it. For this article’s purposes, I will assume that most readers have a basic understanding the employer-sponsored, self-funded health plan.
Understanding that assumptions are dangerous, I will not assume that every reader is an expert, rather, we can all agree that the 100,000 foot, somewhat basic and crass definition of an employer-sponsored, self-funded health plan might be when an employer does not purchase a group product from an insurance carrier, rather it carries the risk associated with its health plan, pays associated health claims out of its own pocket (more or less) and tends to hire lots of vendor solutions to make it all “go.” Again – I acknowledge this is the most basic and 100,000 view of self-funding, but I believe it suffices to serve the rest of this conversation.
Tactics, education and ninjas
Moving on from the assumption that we are now playing in the self-funded space (for purposes of this article) what are some of the immediate tactics that may be employed to push an employer-sponsored plan closer to that “cheap” yet “rich” model?
If a health plan is able to avoid and/or mitigate unnecessary costs whenever possible, that same plan can operate in a very rich manner, gladly paying claims and covering plan members for necessary and needed health costs. By mitigating the unnecessary costs the plan can realign the savings realized distribute plan savings to the membership by reducing the upfront member costs associated with the upkeep of the plan.
A list of tactics – No deep dive here!
Here is a quick list of tactics that are probably not overly novel, or new. The key to success, however, is taking these tactics and assuring that they are operationalized by all parties, adopted (aka “buy in”) by the plan members and plan sponsor, and applied.
Too often, experts in this industry have grand ideas and offer great solutions to solve health plan issues but we do not take the extra step to make sure the solution is truly adopted and accepted by the most important stakeholders – the plan members. It is a familiar story – the one where a health plan solution provider is very excited to sell its solution to a large, new employer-sponsored health plan, yet the solution provider does not go the extra mile to assure buy-in downstream at the employee / plan member level.
The list (disclaimer – this is not an exhaustive list by any means):
- Financial incentives to find billing errors – what if plan members were incentivized, by sharing in the savings, to review their medical bills and EOBs and look for errors!
- Rewards for using cost-containment solutions – what if plan members received a $50 gift card to a huge, online retailer, simply for visiting HR and inquiring about solutions that may exist to guide him/her on their healthcare journey!
- Reference-based-pricing for out of network claims, alone!
- Reference-based-pricing for all claims!
- Patient advocacy & balance billing defense – what if an RBP platform was vigorously supported by robust patient advocacy and balance billing defense to “quiet the noise” so often experienced on RBP platforms!
- Rewards for utilizing preferred providers – what if plan members had diapers and wipes delivered to their doorstep, for a year, simply because they chose a certain hospital to have their baby!
- Zero co-pay / out-of-pocket costs for utilizing preferred providers – what if plan members had all costs waived simply for utilizing an independently owned imaging facility!
- Rx solutions – what if plan members were texted, real-time, as Rx claims were submitted with alternative, more affordable Rx options!
- Medical concierge services – what if plan members actually used these platforms…
- Subrogation – for real – what if a health plan really, really paid attention to their subrogation and recovery efforts and the plan members understood what subrogation was all about!
Plan member incentives – Create a culture of consumerism
When plan members have a vested interest in the performance of their health plan, the members become an integral part of the financial success of that plan.
We must educate our plan members on their health plans and we must assure they are buying in to the utilization philosophies that back their health plans. How often does a reference-based-pricing platform fail because plan members are balance billed and they have never been offered education on what a balance bill is or why their health plan might be using reference-based-pricing.
How often does a concierge service fail to drive plan members toward the most affordable care option because plan members had no idea the concierge service existed! I will never suggest that the casual employee, plan member must become an expert on complicated mechanisms like reference-based-pricing, but it is clear that there must be at least basic education presented at a lunch & learn, or via video on the company website, or through written collateral mailed to all employees, and then reiterated again, and again. Education is key.
To further the efforts of plan member buy in and education, employers should consider doing away with the “one shot” benefits fair prior to open enrollment. Employers should be holding numerous meetings with incentives to drive engagement. Consider the types of employees and what speaks to them – should communication be digital, or should numerous lunch & learns be held? Should the innovative solutions within the health plan be mentioned every month at staff meetings? Could a plan member be featured every month in the company newsletter with a success story on how he or she received such great care while utilizing innovative plan solutions? Could the company highlight how the plan savings will result in a larger bonus pool, or stand up desks for everyone, or a bigger company picnic? Could the employer provide incentives to attend numerous learning sessions – gift cards, extra PTO etc.!
The Ninja
I have spoken on the idea of “The Ninja” at health benefit conferences and meetings all across the United States for at least 2 years now. “The Ninja” was not my idea, so I will not take credit. Rather, I was able to see this concept in practice and I chose to start calling it, “The Ninja.” Instead of picturing a stealthy, assassin-like figure in black pajamas, here is what we are talking about – The Ninja is an HR professional working for the employer who has chosen to sponsor a self-funded health plan. The Ninja may not have a background in human resources, but The Ninja absolutely has a background in healthcare, health claims, cost containment, self-funding, and the like. The Ninja may even come from inside a hospital, a network, a large carrier, a sophisticated consulting shop, or a TPA. The Ninja’s sole purpose is to focus on the application and performance of the employer’s self-funded health plan. The Ninja is able to remove this burden from the HR Generalist who was likely enjoying life and was one day thrown a complete curveball when the CEO said, “Steve, I talked with our insurance broker and he said self-funding is the way to go. So… we’re going to do that. Make it work, Steve!”
It is key to note that The Ninja is not a threat to Steve, nor is The Ninja a threat to the employer’s insurance broker/consultant. To the contrary, if The Ninja is doing her job, she will see that the consultant’s solutions are implemented and performing; she will see that the plan member employees understand their health plan and understand the innovative tools at their disposal; The Ninja will see that Steve, the HR Generalist, is able to do his job and focus on labor issues and people issues unrelated to such a niche area of expertise.
In short, The Ninja will assure that the health plan is performing at a level that will allow for innovative program utilization, the realization of plan savings, the reduction of unnecessary medical costs, and the application of those savings back to the employee plan member. In other words, The Ninja helps make the cheap, rich plan a reality.
Lastly, it should be noted that The Ninja is likely a highly paid employee. And, she should be. Remember, if The Ninja is able to assure that the health plan is performing and that the plan members are using the tools presented, The Ninja’s salary will be a mere splash in the pond compared to the net savings realized by her involvement.
Buy in – The whole point
Ultimately we are talking about a few key ingredients to make this work: a self-funded platform; innovative solutions; full implementation of those solutions; and, most importantly, plan member buy-in and adoption.
I am hopeful that there is nothing in this article that strikes you as overly new, or “innovative,” in terms of the solution platforms discussed. However, I am equally (actually, likely more) hopeful that the ideas of truly gaining buy-in from the plan members and making education a top priority, and/or The Ninja, might be ideas worth exploring to assure that these “old” solutions actually stick and create impact.
At the end of the day, if you have an employee population that understands its health plan and is willing to apply the innovative principles and solutions presented, you very well may have an employer plan sponsor who has been put in a financial position to reduce member-facing plan costs so dramatically that the employee plan member will tell everyone he or she meets, “I will never leave my job – I have the BEST health benefits ever.”
Remember why we do it.
Tim Callender, Esq., serves as the vice president of sales and marketing for The Phia Group. Before joining The Phia Group, Tim spent years functioning as in-house legal counsel for a third party administrator. Tim is well-versed in complex appeals, direct provider negotiations, plan document interpretation, stop-loss conflict resolution; keeping abreast of regulatory demands, vendor contract disputes, and many other issues unique to the self-funded industry.
Read more:
"do it" - Google News
November 20, 2020 at 10:01PM
https://ift.tt/35SUUyZ
Remembering why we do it: Employer-sponsored health plans - BenefitsPro
"do it" - Google News
https://ift.tt/2zLpFrJ
https://ift.tt/3feNbO7
Bagikan Berita Ini














0 Response to "Remembering why we do it: Employer-sponsored health plans - BenefitsPro"
Post a Comment